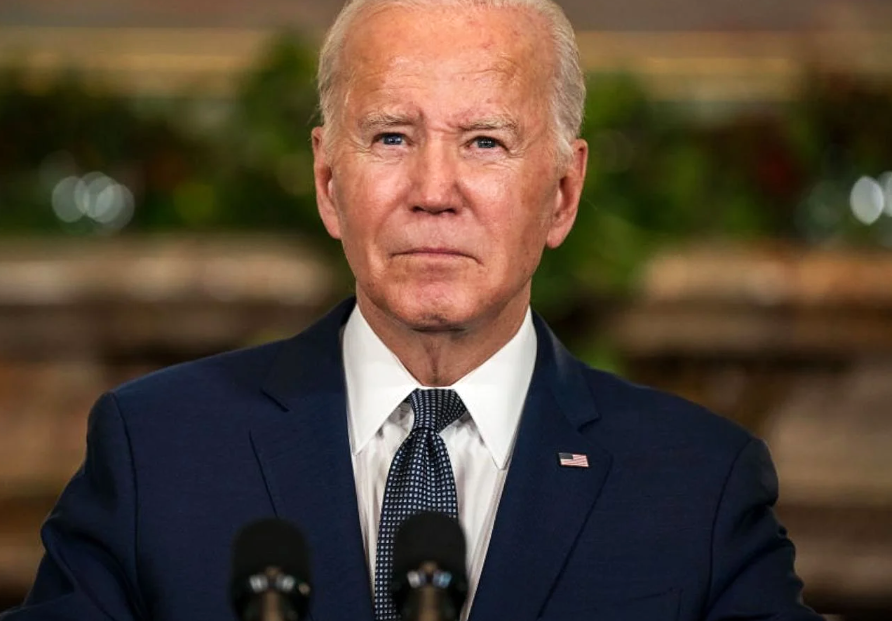
Former President Joe Biden’s cancer diagnosis: What does a Gleason score of 9 mean?
Understanding the Gleason Score in Prostate Cancer Diagnosis
When it comes to diagnosing and evaluating prostate cancer, one of the most critical tools used by healthcare professionals is the Gleason Score.
Developed by pathologist Donald Gleason in the 1960s, this scoring system helps assess the aggressiveness of prostate cancer by examining the microscopic appearance of prostate tissue.
What Is the Gleason Score?
The Gleason Score is a grading system used to evaluate the pattern and structure of prostate cancer cells under a microscope.
It is based on how much the cancer tissue differs from normal prostate tissue. The more abnormal the cells appear, the more aggressive the cancer is likely to be.
How Is the Gleason Score Determined?
A pathologist assigns a Gleason Score after analyzing a prostate biopsy sample. The score is the sum of two grades:
Primary Grade: The most common cell pattern observed.
Secondary Grade: The second most common pattern.
Each grade ranges from 1 to 5, with 1 being the most similar to normal tissue and 5 being the most abnormal.
These two grades are then added together to produce a total Gleason Score between 6 and 10 (scores below 6 are rarely used in modern clinical practice).
Examples:
Gleason 6 (3+3): Cancer cells look similar to normal cells and are usually slow-growing.
Gleason 7 (3+4 or 4+3): Intermediate-grade cancer; the order of the numbers matters—4+3 is considered more aggressive than 3+4.
Gleason 8–10: High-grade cancer; cells are very abnormal, and the cancer is more likely to grow and spread quickly.
Gleason Grade Groups
To simplify interpretation, the Gleason Score is now often translated into Grade Groups:
Gleason Score Grade Group Cancer Aggressiveness
6 (3+3) 1 Low
7 (3+4) 2 Favorable intermediate
7 (4+3) 3 Unfavorable intermediate
8 (4+4, 3+5, 5+3) 4 High
9–10 5 Very high
Why the Gleason Score Matters
The Gleason Score plays a crucial role in determining:
Treatment options (e.g., active surveillance vs. surgery or radiation)
Prognosis (likelihood of recurrence or metastasis)
Need for additional testing (like MRI or genomic testing)
By assessing how aggressive the cancer is, doctors can tailor treatment plans to balance effectiveness and quality of life.
Limitations and Considerations
While the Gleason Score is a valuable tool, it is not the only factor in prostate cancer management.
Other considerations include:
PSA (Prostate-Specific Antigen) level
Tumor stage (based on imaging and physical exam)
Patient’s age and overall health
Genetic and molecular markers (in some cases)
Conclusion
The Gleason Score remains a cornerstone in the diagnosis and management of prostate cancer.
By grading the appearance of cancer cells, it provides insight into the tumor’s behavior and guides personalized treatment decisions.
Ongoing research continues to refine this system and integrate it with emerging biomarkers to improve outcomes for patients.



